The human hand is a marvel of biological engineering, capable of performing tasks that require incredible precision and strength. For pediatric occupational therapists, understanding the intricate anatomy and function of the hand is essential when screening for reflex patterns such as the Palmar Grasp, Babkin Reflex, and Hands Pulling Reflex. This foundational knowledge allows therapists to assess movement holistically and design interventions that are both effective and tailored to each child’s unique needs.
Why Hand Anatomy Matters
The human hand consists of 27 bones, more than 20 joints, and approximately 30 muscles. These structures work together to allow complex movements such as gripping, pinching, and manipulating objects. Pediatric occupational therapists often encounter children with fine motor delays, which may manifest as challenges in tasks like handwriting, using utensils, or manipulating small objects. However, fine motor skills go beyond these common goals—they are critical for developing independence, cognitive skills, and even emotional expression.
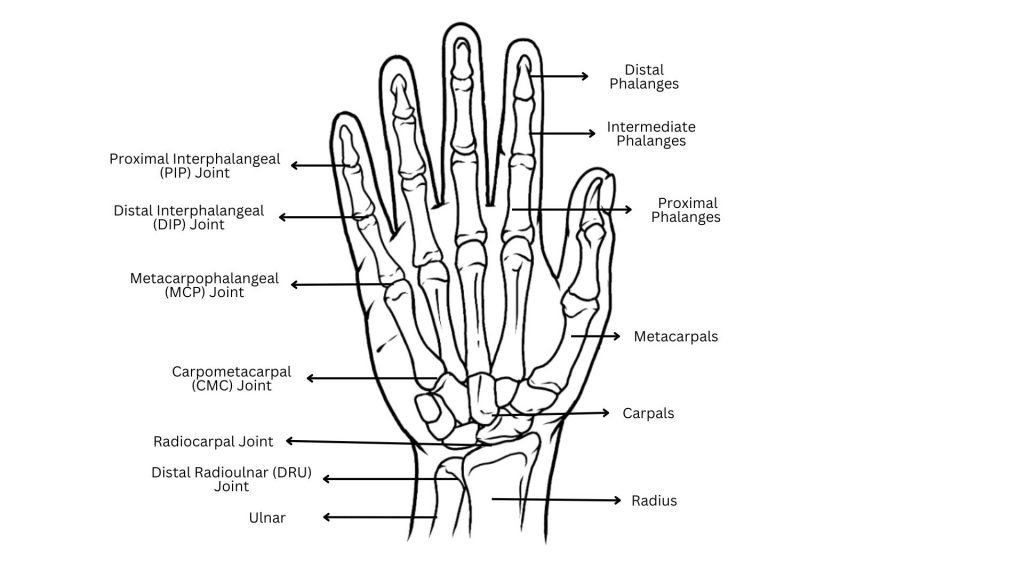
Each reflex pattern influences how these anatomical components function and interact during developmental stages. For instance:
- Palmar Grasp Reflex: This reflex involves an automatic curling of the fingers when the palm is stimulated. Persistence of this reflex beyond infancy can indicate developmental delays or neuromotor dysfunction.
- Babkin Reflex: Stimulating the palms can cause mouth opening or head movements, highlighting a connection between hand and oral motor development. This connection can influence feeding, speech, and even early social interactions.
- Hands Pulling Reflex: This reflex facilitates the activation of core and upper limb muscles, forming a basis for controlled reaching and grasping.
Understanding the role of these reflexes in hand function allows therapists to screen for underlying challenges in coordination, strength, and sensory integration.
Beyond Handwriting and Shoe-Tying: Recognizing Comprehensive Goals
Fine motor development affects every area of a child’s life. Consider tasks like self-care, feeding, or participating in school activities. Children with fine motor delays might struggle with buttoning clothes, opening lunch containers, or using scissors during art projects. Therapists must recognize the broader implications of fine motor challenges, which include:
- Social Participation: Children may avoid group activities or play that requires manual dexterity, affecting their confidence and peer relationships.
- Academic Success: Difficulty in tasks like cutting, pasting, or writing can hinder academic engagement and performance.
- Sensory Integration: Challenges with fine motor skills often overlap with sensory issues, making it harder for children to process and respond appropriately to tactile stimuli.
Recognizing Compensatory Patterns
A deep understanding of hand anatomy enables therapists to identify compensatory movement patterns that may mask underlying reflex retention. For example:
- Difficulty Differentiating Right and Left Sides: Struggles with recognizing and coordinating the right and left sides of the body can indicate broader coordination challenges. This difficulty may hinder activities that require crossing the midline, like zipping a jacket or tying shoes.
- Challenges with Alternating Hand Movements: Difficulty alternating hand use, such as in activities like drumming or bilateral cutting, may force both hands to work in unison rather than independently, reducing efficiency and dexterity.
- Mouth Opening and Closing with Hand Opening and Closing Pattern: This pattern reflects a connection between oral and manual motor systems. Retained reflexes can lead to challenges in isolating these movements, which are critical for fine motor tasks like feeding and speech development.
By assessing these patterns, therapists can differentiate between developmental delays stemming from reflex pattern retention and those caused by structural abnormalities or muscle imbalances. Addressing these compensations early prevents further challenges and ensures smoother developmental progress.
Screening Strategies
Pediatric therapists can incorporate the following approaches to screen for reflex-related challenges effectively:
- Functional Movement Assessments: Evaluate how a child manipulates objects during play to identify inefficiencies in grip or hand positioning. Watching a child stack blocks, manipulate small toys, or build with Legos can provide invaluable insights.
- Tactile Stimulation Tests: Check how the palms and fingers respond to touch to see if reflex patterns are still present. Use different textures, gentle vibrations, or light pressure to test sensitivity and how reflexes react.
- Fine and Gross Motor Integration: Observe how hand movements coordinate with larger muscle groups during tasks like crawling, climbing, or writing. Many fine motor issues stem from weaknesses in proximal stability, making core and shoulder assessments vital.
Therapists who pair their knowledge of anatomy with these strategies can create a strong foundation for accurate screening and intervention. Recognizing that fine motor skills are part of a broader developmental system allows therapists to create comprehensive, individualized treatment plans that empower children to succeed in all aspects of life.